Prevention and control should be at the center of NCD care to reduce the susceptibility of those at risk and to ensure the healthy remain healthy.
– Dr. Bachani. Former Deputy Commissioner of NCDs, Ministry of Health, India
According to the World Health Organization, non-communicable diseases (NCDs) —including diabetes, cardiovascular diseases, and cancers—are the leading cause of death globally and responsible for 70% of deaths worldwide. No longer diseases of the “predominantly rich,” NCD prevalence is increasing most markedly in low-and middle-income countries (LMICs), where more than 75% of global deaths occur. This places a double burden on health systems in these countries which are already strained by infectious diseases. Halting and reducing the burden of NCDs in LMICs will require significant investment across all health system components, particularly at the primary health care level.
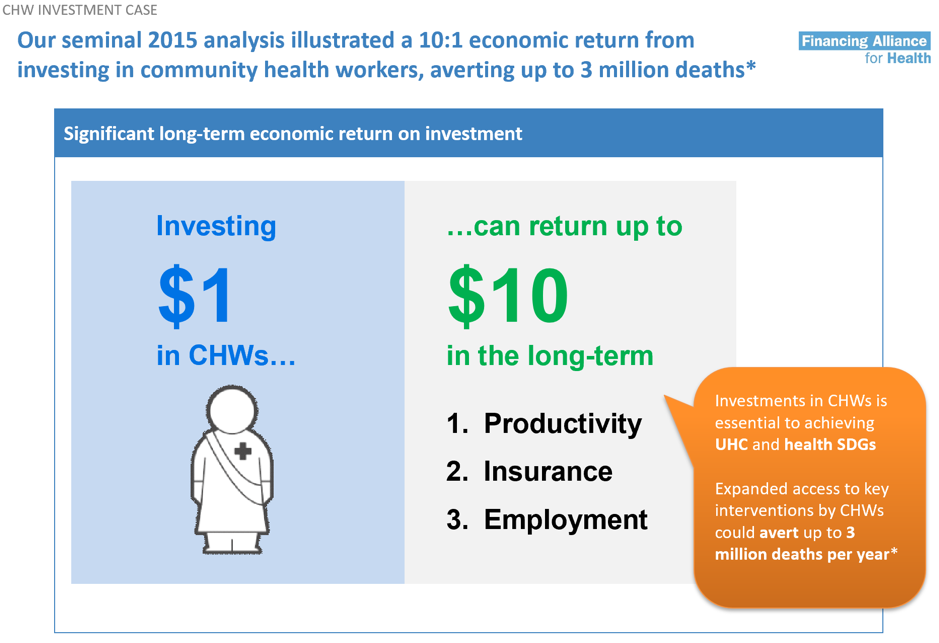
For a significant proportion of people in LMICs, community health is a frequent entry point into the health system. Therefore, strengthening community health as part of broader primary health care, is integral in the response to NCDs. Community health workers (CHWs)—members of a community trained to deliver basic health services—provide a range of services from maternal and child health, family planning, nutrition, and disease surveillance to diagnosis and treatment of malaria and HIV. Moreover CHWs have been shown to be a cost-effective way to extend health services to the hardest-to-reach communities. An analysis by the Financing Alliance for Health found a 10:1 return on investment for community health when accounting for averted mortality, avoidance of high costs of health crises, and the economic impact of increased employment.
Increasingly, it is being recognized that CHWs could be leveraged to deliver NCD services, including prevention, early diagnosis and management, in conjunction with the services they traditionally offer. According to Arnaud Bernaert, a Senior Director of the World Economic Forum, “when you send health care workers to the house of patients to test for HIV, why not also test for high blood pressure and glucose levels? The moment that connection exists because of community proximity, it should be leveraged beyond the traditional program…you can do so much more with that interaction.”
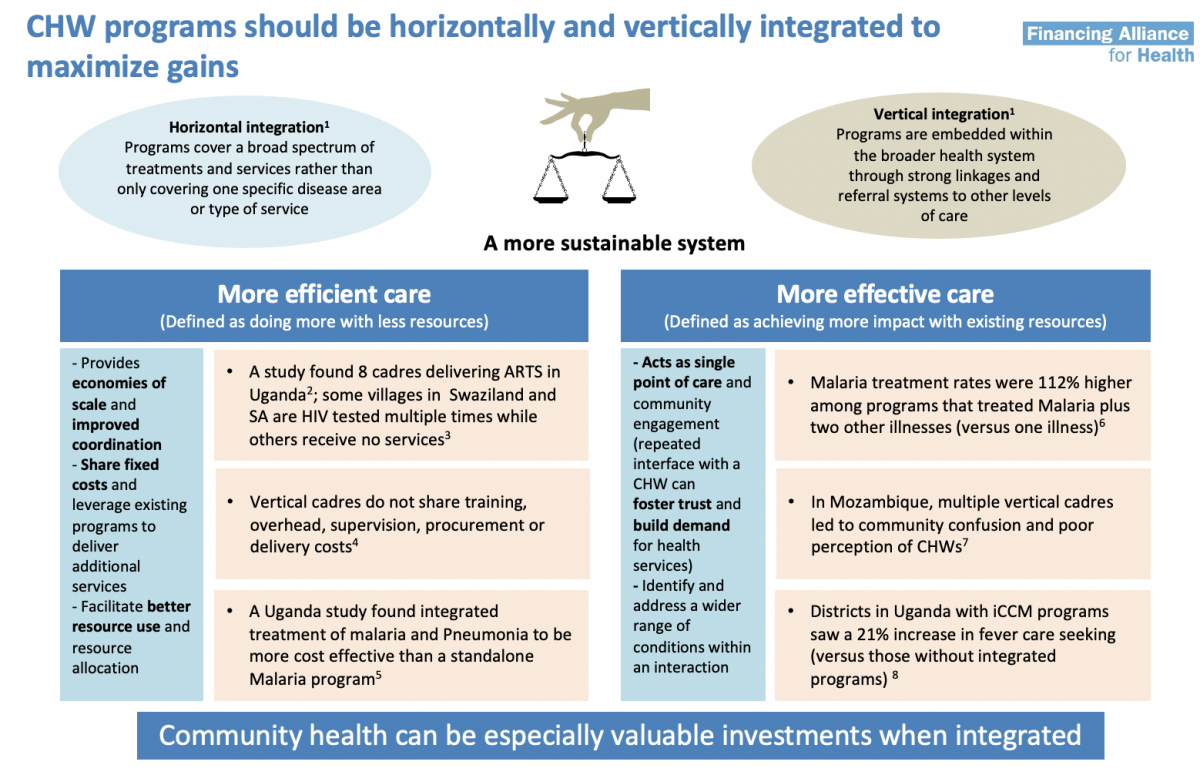
The potential benefits of such integration are significant: it can allow for more efficient care provision through economies of scale, improved coordination, sharing of fixed costs, and better use of resources. Additionally, it can ensure more effective health services through repeated interaction, which fosters trust and builds demand for health services, and enables a wider range of conditions to be addressed with a single interaction.
However, the cost and cost effectiveness of integrating NCD services to existing packages of community health services needs to be established. The Financing Alliance for Health, with the support of Medtronic Foundation, attempted to answer this question. The analysis found that there is currently very limited data, particularly on long term health outcomes and on costs, restricting the ability to draw crucial insights on the costs and cost-effectiveness of NCD integration. More granular data is needed to understand cost drivers and how the cost structure for integrated NCD programs compares with that of traditional CHW interventions. Also, further research is needed to understand the optimal role, number, and types of NCD care activities to be incorporated into CHW packages in different contexts, their operational enablers, and impact on health outcomes.
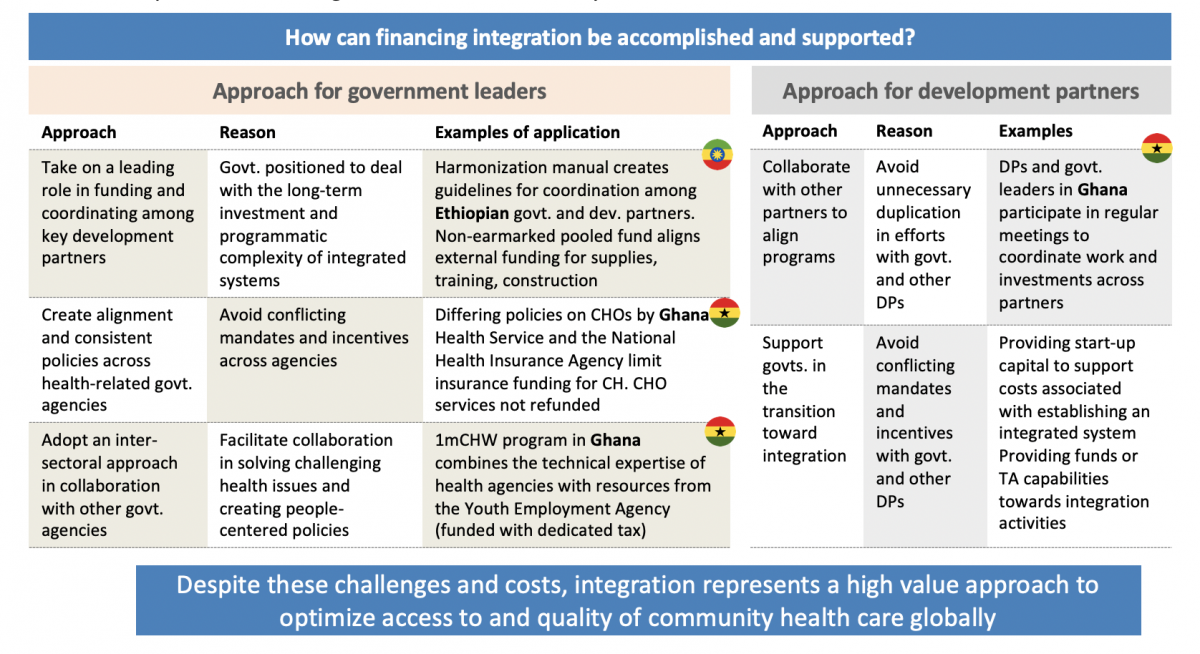
Financing—which is the most enduring obstacle to strengthening health systems in many countries—represents a major challenge for integrating NCD services into community health worker activities. This requires a complete rethink of how government leaders budget, engage with and coordinate development partners, and organize roles and responsibilities throughout the broader health system.
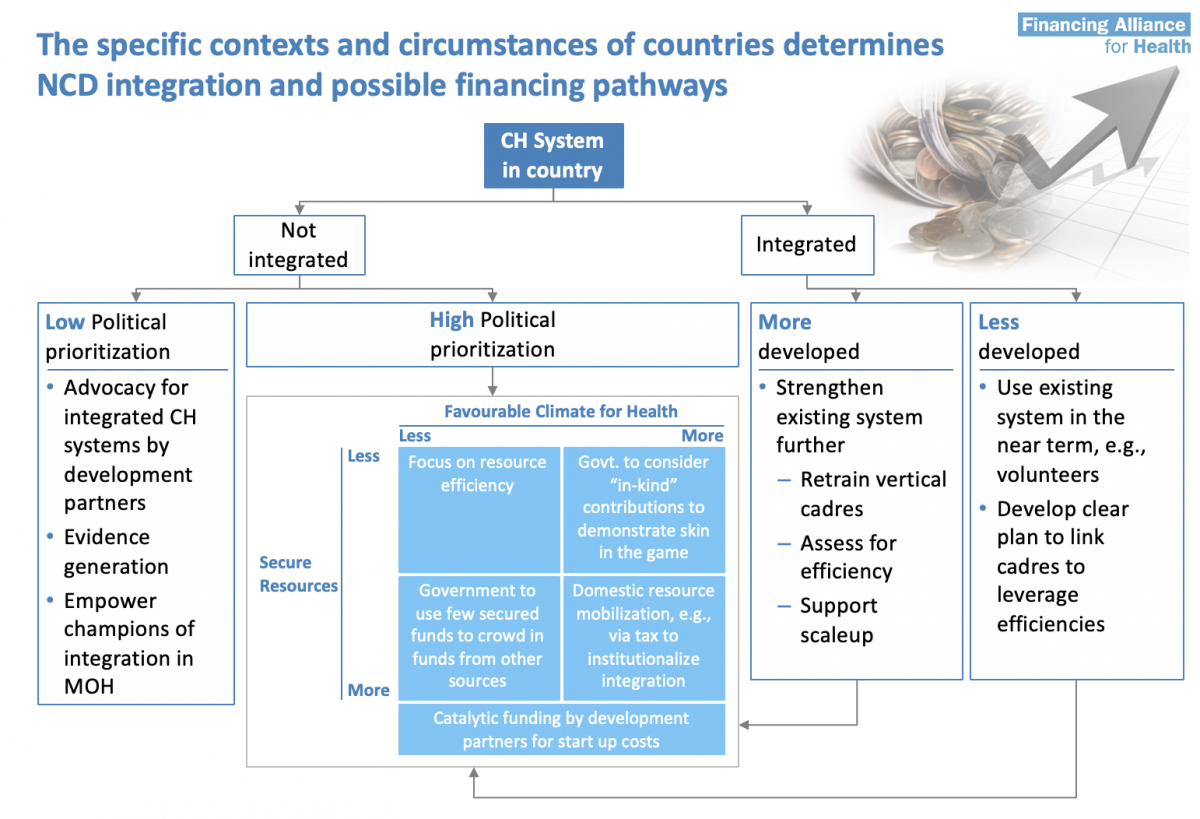
Different countries can take different approaches toward NCD integration based on each country’s existing community health system (e.g., starting from scratch verses existing highly vertical cadres verses existing integrated systems), financing mechanisms, and broader socio-political contexts.
Despite these challenges, integrating NCD services into community health represents a high value approach to optimize access to and quality of health care for developing countries. At the heart of this, will be the community health workers who are crucial to delivering these improved health outcomes!




